From the basic "conduction road map" of the heart, seen in Figure 1, we can start illustrating concepts.
 |
| Figure 2: The sinoatrial node depolarizes and the depolarization wavefront travels rapidly along the internodal pathways and Bachmann's Bundle, towards the atrioventricular node and the left atrium. |
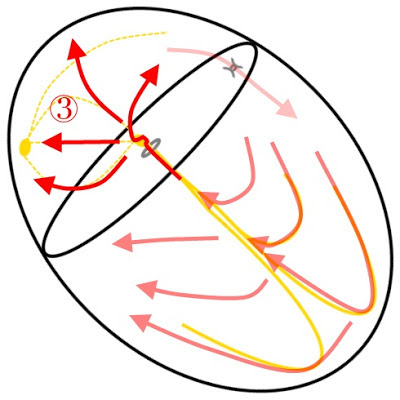
Beginning in Figure 2 and continuing through Figure 4, we can see the propagation of a depolarization wavefront started in the sinoatrial node and its eventual path through to the bundle branches. While difficult to express on an actual whiteboard, fading of the older impulses is used to help represent the time component of the signal.
Reentrant Tachycardias
The beauty of this style of drawing is the ability to convey concepts such as Atrioventricular Nodal Reentry Tachycardia (AVNRT). A certain subset of the population has two or more distinct zones of conduction in their AV node. Often there are dual pathways with one of the zones conducting impulses quickly but recovering slowly, and the other conducting impulses slowly and recovering quickly.In a sinus rhythm this difference in conduction through the atrioventricular node is not apparent. However, if a well timed premature atrial contraction (PAC) is present, this dichotomy can be exploited. In Figure 5 we can see the sinus impulse arriving at the AV node, with part of the wavefront traveling through the fast pathway, and part of the wavefront traveling through the slow pathway.
Continuing in Figure 6, the slow pathway with its shorter effective refractory period, begins recovering quicker than the fast pathway. Once through the AV node the depolarization wavefront continues through the Bundle of His and into the bundle branches and Purkinje fibres as during normal conduction.
 |
| Figure 6: The dichotomy of recovery in the two atrioventricular nodal pathways are illustrated. |
It is at this vulnerable point that a well timed extrasystole can take advantage of the heterogeneous repolarization of the AV nodal pathways. Figure 7 depicts the initiation of a PAC which reaches the slow pathway while it is completely recovered and the fast pathway is still absolutely refractory.
In Figure 8 we can see the "rotation" of reentry initiated as the depolarization wavefront travels forward (antegrade) through the slow pathway and backwards up (retrograde) the fast pathway which has now recovered. Impulses are then distributed down through the Bundle of His each time the rotation through the slow pathway reaches the insertion of the Bundle of His. It is this reentry, best illustrated as a rotation, that not only initiates the tachycardia but sustains the tachycardia as well.
When viewing Figure 8, you may see why typical AVNRT results in a Pseudo-S wave in Lead II (Figure 9) and Pseudo-R' wave in Lead V1, as once the tachycardia begins the impulses are conducted to the atria retrogradely from the fast pathway. Ventricular depolarization continues as it would during normal conduction, using the normal ventricular conduction tissues for propagation.
 |
| Figure 9: The Pseudo-S wave, highlighted in red, seen during typical atrioventricular nodal reentry tachycardia as the atria are depolarized retrogradely. |
Reentry Outside the AV Node
Atrioventricular nodal reentry is not the only means of reentrant tachycardias. Less than 1% of the population features an extra "exit" in their conduction road map, known as an Accessory Pathway (AP, featured in Figure 10) or an Accessory Bypass Tract.Drs. Wolff, Parkinson, and White were the first to describe a series of patients featuring bundle branch blocks and a short PR intervals who suffered from paroxysms of tachycardias in the 1930's. However, it was not until the late 1940's that these abnormalities were isolated by Drs. Ohnell and Wood as bundles of conducting tissue which connected the atria and ventricles, independent of the AV node.
AV nodal tissue features the property of decremental conduction; simply stated, it acts as a speed bump slowing the conduction of a depolarization wavefront. The upper limit of atrioventricular conduction is often less than 220 bpm although this varies with age. Typical accessory bypass tracts do not feature decremental conduction and can often conduct both antegrade and retrograde signals in excess of 220 bpm.
The hallmark feature of an AP is pre-excitation of the ventricles. As sinus impulses arrive at both the AV node and the AP, illustrated in Figure 11 and Figure 12, the depolarization wavefront is slowed in the AV node but conducted without delay through the AP.
 |
| Figure 11: A sinoatrial node depolarization travels towards the AV node and an Accessory Pathway (AP). |
Figure 12 shows that ventricular myocardium begins depolarizing as the AP terminates directly into ventricular tissue.
In Figure 13, this direct connection to ventricles pre-excites some myocardium while normal conduction through the bundle branches from the AV node occurs.
 |
| Figure 13: As depolarization of the ventricles continues, the two wavefronts meet. The fusion of these two wavefronts often mimics a bundle branch block. |
 |
| Figure 14a: Comparison of the QRS morphology during a sinus rhythm and a sinus rhythm with pre-excitation through an accessory pathway. |
Reentry Using an Accessory Pathway
If pre-excitation were the only feature of an accessory pathway, Wolff-Parkinson-White would exist merely as a fascinoma. However, as previously noted, most accessory pathways are pathological featuring non-decremental antegrade and retrograde conduction.This additional circuit may join with the AV node and be exploited by extrasystoles or heterogeneous repolarization. This class of tachycardias is known as Atrioventricular Reciprocating Tachycardia (AVRT) or the older Circus Motion Tachycardia (CMT).
Orthodromic Reentry
AVRT is divided into two types based on the direction of travel in the circuit. Orthodromic AVRT occurs when the reentry is antegrade through the AV node then retrograde through the AP; thus conduction through the ventricles proceeds normally. An orthodromic circuit can be initiated by a premature ventricular contraction (PVC) or blocked antegrade conduction through the AP.Figure 15 illustrates the arrival of a sinoatrial depolarization at both the AV node and the AP, with forward conduction through the AP blocked.
 |
| Figure 15: A sinoatrial depolarization arrives at the atrioventricular node and an accessory pathway, finding the AP blocked. |
 |
| Figure 16: Conduction proceeds normally through the AV node. |
 |
| Figure 17: As the ventricles depolarize and conduction continues through the ventricles the wavefront finds that retrograde conduction through the AP is not blocked, contrary to antegrade conduction. |
Antidromic Reentry
In Antidromic AVRT, conduction of the reentry circuit begins antegradely through the accessory pathway and completes retrogradely through the atrioventricular node. Because ventricular depolarization does not begin with the normal ventricular conduction network, antidromic AVRT will present as a regular wide complex tachycardia due to slower propagation of ventricular depolarization.As in orthodromic AVRT, an antidromic circuit can begin with an extrasystole or with blocked conduction. In Figure 19, a PAC travels forward through the atria entering an accessory pathway and is concurrently blocked by a refractory AV node.
 |
| Figure 19: An atrial extrasystole finds the AV node refractory, however, is able to conduct antegrade through an accessory pathway into the ventricles. |
 |
| Figure 20: Activation of the ventricular myocardium begins outside the conduction network and eventually reaches the AV node. |
 |
| Figure 21: Retrograde depolarization of the AV node and atria occurs. The accessory pathway does not feature the decremental conduction seen in the AV node and is already completely repolarized. |
Atrial Fibrillation and Wolff-Parkinson-White
Unfortunately, reentry rhythms are not the only means of tachycardias utilizing an accessory pathway. If an automatic atrial focus were to have access to a non-decremental accessory pathway the results will be rapidly fatal. Many patients with Wolff-Parkinson-White will experience episodes of atrial fibrillation (AF). In atrial fibrillation, numerous atrial wavefronts are present producing cyclic rates of 400-800 bpm.Atrial fibrillation and WPW is characterized by varying degrees of fusion between antegrade conduction of f-waves through the AV node and the AP. This is seen on the surface ECG as a rapid, grossly irregular tachycardia with alternating QRS morphologies ranging from narrow to very wide.
Figure 23 features atrial fibrillation wavefronts depolarizing the AV node and encountering a refractory accessory pathway.
 |
| Figure 23: Atrial fibrillation with conduction through the AV node and blocked conduction through an AP. |
 |
| Figure 24: Conduction through the bundle branches and Purkinje Fibres propagates normally and the continued f-waves are blocked at both the refractory AV node and AP. |
 |
| Figure 26: Varying degrees of fusion occur as antegrade conduction proceeds through the AV node and AP. |
I hope my digital reproductions of Whiteboard Cardiology proved useful and drop me a line if you have ideas for other concepts in electrocardiography that would be simplified through line art.
All of these images are free to use and licensed Creative Commons Attribution-Share Alike 3.0, available for download on my Google Drive. The originals were created using Paint.Net.












13 comments:
This is fantastic! Understanding what happens and how it occurs makes it so much more easy to perform ECG interpretation than rogue pattern memorization. I especially like the slides that also featured ECG complexes. That brought it home. More,please!!!
Cardiology is subspecialty of internal medicine and a person who is planning to practice cardiology should go through residency program. cardiology residency length gives specialized practice and training. In the program, you will have the opportunity to learn about preventing, treating and diagnosing conditions and diseases of cardiovascular system and heart.
The gpa problems can overcome a low grade point average by compensating in other areas. The reasons for having a low GPA and the school you are applying to can also be a factor.
Business school essays will be discouraging, as candidates try and decide what to write down regarding and the way to best convey their experiences and enthusiasm to the master's degree admissions committee. internship motivation
The abilities of the doctor of this hospital are unbelievable and working so hard. The transplant is one of the difficult things and you have to examine every part of the body but sample eras application provides nice job. Helen is under the process of the transplant and doctors are working so well.
Good day I am so glad I found your website, I really found you by error, while I was browsing on Bing for something else, Anyhow I am here now and would just like to say thanks a lot for a fantastic post and a all round thrilling blog (I also love the theme/design), I don’t have time to read through it all at the minute but I have bookmarked it and also added in your RSS feeds, so when I have time I will be back to read a lot more, Please do keep up the awesome work. find a cardiologist in london
Learning electrocardiography is explained with white board method is really easy to study. Consult good cardiologist near you in cardiac difficulties.
nice information.Doctoriduniya
Nice explanation about white board cardiology.
Best Cardiologist London
well written health blog it is very informative , follow Meddco healthcare https://www.meddco.com/ for the best health treatments and and affordable diet plans
Thank you because you have been willing to share information with us. we will always appreciate all you have done here because I know you are very concerned with us.
Regards,
Cardiologist near me
Thank you for the insightful illustrations and explanations on electrocardiography. It’s fascinating to see how well concepts like AVNRT and accessory pathways are explained through visual depictions. For more information on heart conditions and treatments, you might find Dr. Manish Juneja’s work invaluable. His expertise in cardiology can offer further insights into heart health. Check out Dr. Manish Juneja for more details. Great content here!
Post a Comment